A Guide to Medicare Dual Eligible Special Needs Plans (D-SNPs)
A Medicare Dual Eligible Special Needs Plan (D-SNP) is a type of Medicare Advantage Plan that is only available to a specific subset of Medicare enrollees. More broadly, Special Needs Plans (SNPs) provide coverage to people with specific diseases or circumstances. Dual Eligible Special Needs Plans are set up to help ensure that people experiencing financial hardship have access to the medical care they need.
What is a Dual Eligible Special Needs Plan?
A Medicare D-SNP is available to people who have both Original Medicare and Medicaid. You must maintain your eligibility for both of these programs to stay enrolled in a D-SNP. Not all carriers or regions offer Dual Eligible Special Needs Plans, so check with an expert if you think you may be eligible for enrollment.
Losing your Medicaid eligibility means you will be disenrolled from the D-SNP. After your eligibility lapses, you have a grace period before your coverage ends to reestablish that you meet Medicaid’s requirements. Medicare requires that this grace period lasts at least a month, though some plans may have a larger window.
If you are not able to re-enroll in Medicaid, you aren’t out of options! You enter a Special Enrollment Period (SEP) when you receive notice that you are no longer Medicaid eligible. The SEP runs through your D-SNP’s grace period, and for 2 months after your coverage ends if you are unable to re-enroll. During this time, you can shop for another plan to make sure you are never without coverage.
What Benefits do D-SNPs Provide?
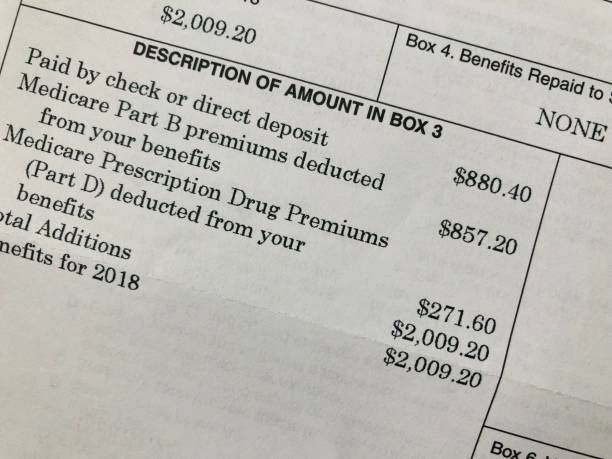
Dual Eligible Special Needs Plans cover the same care as Medicare Advantage Plans. This includes hospital insurance, medical insurance, and prescription drug coverage. D-SNPs also provide additional benefits at no cost to you like dental, vision, and hearing care. Since these plans are designed for people with limited financial resources, most healthcare costs are covered between the Original Medicare and Medicaid components.
Individuals enrolled in D-SNPs also receive benefits to offset the cost of everyday necessities. Some plans offer up to $165 a month in over-the-counter medicine and healthy food allowances. This benefit is designed to help enrollees buy essential health and grocery items. In addition, there are D-SNPs that include flex spending cards for dental, vision, and hearing costs not specifically covered by the plan.
What is a Care Coordinator?
Another benefit provided by D-SNPs is a care coordinator. These skilled professionals work to help you access all of the resources available to you. It can be tough to navigate the benefits you receive through Medicare and Medicaid, not to mention other programs within your community. The care coordinator’s goal is to keep you informed and help you make the best use of these services. Taking advantage of every healthcare benefit at your disposal is a great way to keep you in the best health possible!
Not everyone needs a Dual Eligible Special Needs Plan, but this kind of coverage is incredibly valuable for those who need it. If you have Medicaid and will soon be eligible for Medicare coverage, we’d love to hear from you! Senior Insurance Advisors will always work hard to make sure you understand your options and empower you to make the best decisions for your Medicare coverage.