A Medicare Special Enrollment Period (SEP) provides an opportunity to change your Medicare coverage when your life changes significantly. Your unique situation determines what Parts of Medicare you can change and how long you have to do so. Unlike most other Medicare Enrollment Periods, SEPs generally do not fall during a set time of year. We’ve chosen to highlight some common life changes that can result in Special Enrollment Period eligibility.
Qualifying Life Events While Already Enrolled in Medicare
For people already enrolled in Medicare, a qualifying life event provides a chance to change your Medicare Advantage or Part D prescription drug plan. You may be eligible to make changes under a Special Enrollment Period if you move, your plan’s contract changes with Medicare, or you have an opportunity to enroll in coverage other than Medicare. Qualifying life events most commonly initiate a 2-month Special Enrollment Period. Your Medicare advisor will be able to confirm both when you enter an SEP and how long you have to make changes to your coverage.
Joining Medicare After Losing Creditable Employer Coverage
If you worked past age 65 and delayed Medicare enrollment due to creditable employer coverage, you are eligible to enroll in Medicare during a Special Enrollment Period. You have 8 months from when you leave your job or your employer ends your creditable coverage to enroll in Original Medicare.
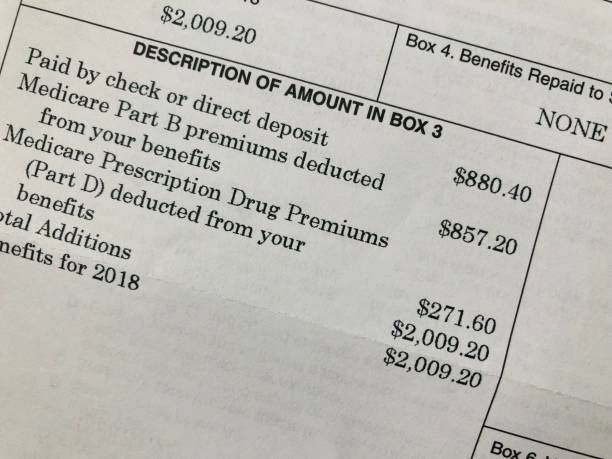
Decisions about joining a Medicare Advantage Plan or enrolling in Part D prescription drug coverage, though, must be made in the first 2 months from your loss of employer coverage. This smaller, 2-month window also applies to people whose employer coverage was previously creditable but isn’t any longer. Delaying enrollment in Medicare Advantage or Part D coverage can result in late enrollment penalties.
How Assistance Programs Impact Medicare SEPs
If you are enrolled in a State Pharmaceutical Assistance Program (SPAP), you may enroll in Medicare prescription drug coverage through an SEP once in a calendar year. This can be either a standalone Part D plan or through a Medicare Advantage Plan. Losing eligibility for your SPAP assistance also opens up this one-time Special Enrollment Period.
Medicare enrollees who also receive Medicaid can change their Medicare Advantage or Part D prescription drug coverage once during each of the Special Enrollment Periods that run from January to March, April to June, and July to September. If you are dual-eligible and lose your Medicaid eligibility, you have a separate 3 month SEP to add, switch, or drop parts of your Medicare coverage.
Similar to Medicaid recipients, Medicare enrollees who qualify for Extra Help have access to Special Enrollment Periods throughout the year. If you’re receiving Extra Help, you can make changes to your Medicare prescription drug coverage during the same quarterly SEPs from January to September of each year.
We can help you understand your options during a Special Enrollment Period so you’re never without the right coverage. When you’re ready, reach out by phone or send us a message. Our trusted advisors are here year-round to let you choose your Medicare coverage with confidence.