Enrolling in Medicare is just the first step in your health insurance journey! One of four annual enrollment opportunities, the Medicare Annual Enrollment Period provides a chance for Medicare enrollees to purchase additional coverage or make changes to an existing plan. We have guided many people through coverage modifications during the AEP and address several common questions we have heard along the way to help you make the best decisions for your own Medicare situation.
When is the Annual Enrollment Period?
Like the name implies, this enrollment period opens up once a year, every year. The AEP begins October 15th and all requested changes must be submitted by December 7th. Medicare plan modifications you make during the AEP take effect January 1st of the following year.
Who is the Annual Enrollment Period for?
Anyone enrolled in a Medicare plan can make changes to their coverage during the AEP. This enrollment period does not serve as a backup for people who need to start their Medicare coverage, and missed out on their Initial Enrollment Period (IEP). If you are a first-time Medicare enrollee, our Initial Enrollment Period Checklist lays out how to prepare for initiating your Medicare coverage.
What changes can I make to my policy?
The changes available to you during the AEP vary based on your current coverage. Depending on your existing Medicare plan, you can make changes like:
- Switching from Original Medicare to a Medicare Advantage plan, or vice versa
- Adding or removing prescription drug coverage within a Medicare Advantage plan
- Joining or dropping a Part D prescription drug plan to/from Original Medicare
- Choosing a different plan from your existing insurance carrier
- Moving to a new Medicare Advantage plan
Do I have to modify my coverage every year?
If you are happy with your current Medicare plan, you are not required to change it during the AEP. In fact, many plans auto-renew January 1st for your convenience.
How do I decide if I need to make changes?
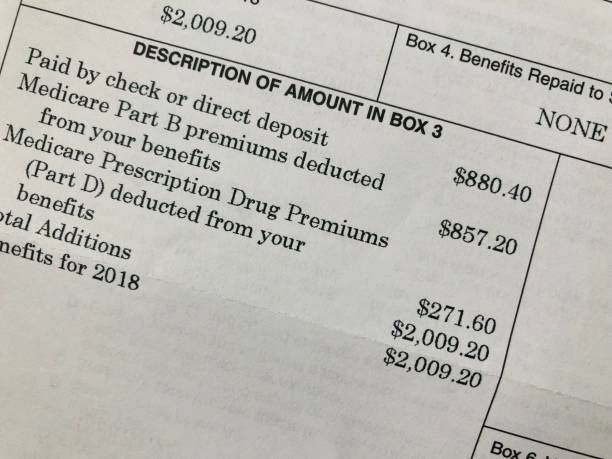
The AEP provides an opportunity for you to assess how your current Medicare coverage has served you over the past year. Think about things like your existing plan’s costs, your budget, how your health has changed, and whether your insurer will be making changes to your plan. Take time to review the Medicare & You handbook for the next coverage year if you have Original Medicare. Individuals enrolled in Medicare Advantage or Part D prescription drug coverage plans should keep an eye out for an Annual Notice of Change (ANOC) and/or Evidence of Coverage (EOC) document from your carrier.
After reviewing these annual disclosures, you may find that your insurer has a different plan better suited to your new healthcare needs, or that it is best to switch carriers entirely. Sometimes you can find a plan with the same coverage at a more affordable cost. The AEP is a great time to comparison shop for your best fit.
I missed the December 7th deadline—what now?
If you are enrolled in a Medicare Advantage Plan, you have another opportunity to make coverage changes during the Medicare Advantage Open Enrollment Period. The MAOEP runs from January 1st through March 31st of every year. Changes made to Medicare Advantage plans during this time period take effect on day 1 of the month following your modified enrollment. For other plan types, there are a few other enrollment period options available to you.
While the Annual Enrollment Period gives Medicare recipients a chance to modify their coverage, plan changes should not be taken lightly. Senior Insurance Advisors has the knowledge to help you make the most informed decisions about your Medicare needs, whether you are a Nebraska native or reside in another of our 8 licensed states. Contact us today to schedule a free, no-obligation consultation or join us at an upcoming community event!